※この記事は、日本に住む外国の方向けに、英語で書かれています。
At Iwata Neurosurgical Clinic (Osaka), we have begun offering an autologous cancer vaccine as a personalised immunotherapy option for patients with glioblastoma, an aggressive malignant brain tumour.
Glioblastoma is the most aggressive primary brain tumour. It can infiltrate normal brain tissue, which makes complete surgical removal challenging.
Current standard of care
The present standard treatment combines surgery, radiotherapy and chemotherapy as a multidisciplinary approach.

Immunotherapy as the “fourth” treatment pillar
Because complete cure is difficult in many cases, controlling disease progression and alleviating symptoms are often important goals. Against this backdrop, immunotherapy is drawing attention as a fourth option.
Immunotherapy harnesses the patient’s own immune system to fight cancer. With the advent of immune checkpoint inhibitors, interest has grown worldwide.
Autologous cancer vaccine uses tumour tissue removed during surgery to manufacture a vaccine designed to trigger immune responses specifically against your own tumour — a form of personalised medicine.
Contents
What is an autologous cancer vaccine?
The vaccine is manufactured from your own tumour tissue removed during surgery and processed using a dedicated technique to induce an immune response. It is positioned as a form of personalised (bespoke) immunotherapy.
Proprietary technology
Fresh tumour tissue is not required. Even tissue removed years earlier can be used if it is available as formalin-fixed, paraffin-embedded (FFPE) blocks stored for pathology. This technology is patent-protected and provided exclusively by Cell Medicine, Inc.
How it works & safety
Mechanism
After vaccination, immune cells learn to recognise tumour-specific markers (neoantigens) and target them. The aim is to enable your immune system to attack microscopic residual cells and potential recurrences or metastases after surgery.
Safety and specificity
The vaccine is intended to direct immune responses towards cancer cells while limiting effects on healthy tissue.
In prior clinical experiences, severe adverse events have not been commonly reported.
Note: because the vaccine stimulates immunity, patients with active autoimmune diseases are generally not eligible.
Steps to receive treatment
Secure your tumour tissue
To proceed, we require your own tumour tissue in FFPE blocks (formalin-fixed or paraffin-embedded).
If you had surgery in the past, those tissues may be available. Please request a loan of the blocks from the hospital where your surgery was performed. If that is difficult, our clinic can assist with the paperwork.
Initial consultation
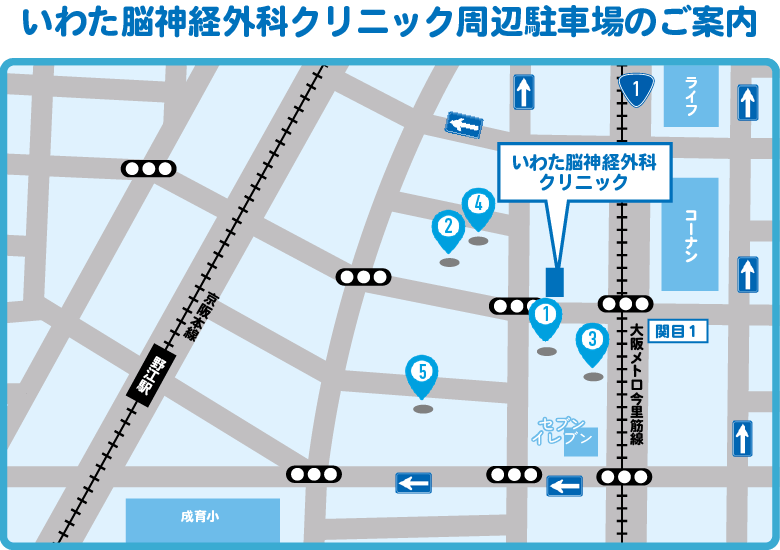
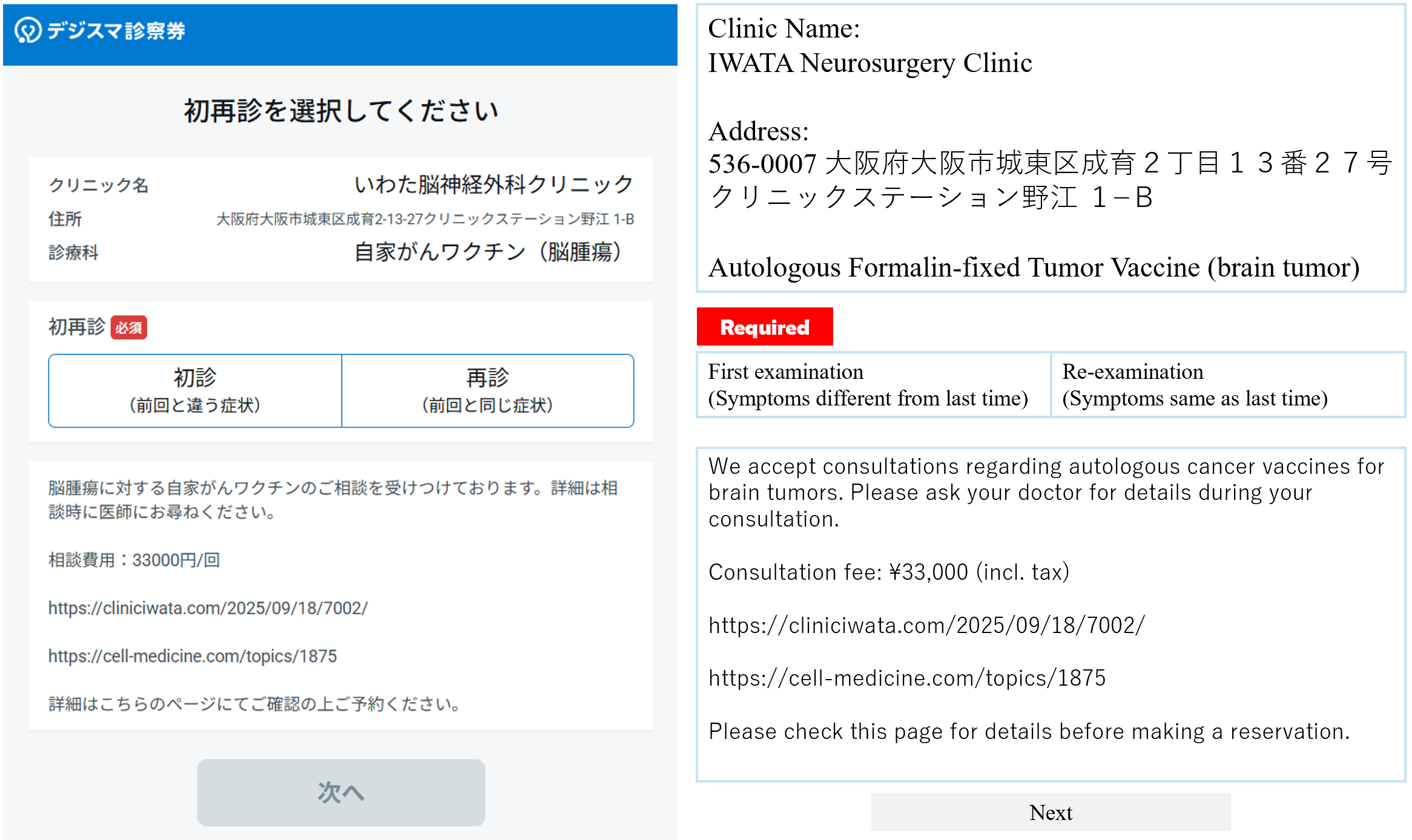
Book your first appointment and bring the secured tissue (or hospital contact details). The doctor will assess eligibility and discuss the treatment plan with you.
You can book at Iwata Neurosurgical Clinic from the link below.
Vaccine manufacturing & administration
From receipt of tissue, vaccine manufacturing typically takes about 1–2 weeks. No hospital admission is required; injections are given in our outpatient clinic. One course consists of 3 vaccinations over approximately 4–6 weeks.
Best timing to start
The ideal timing is post-surgery and before starting chemotherapy, when the number of residual cancer cells is presumed to be low. Combination with radiotherapy, selected chemotherapies and immune checkpoint inhibitors may be possible. Patients with markedly reduced general condition may be ineligible.
Costs
The autologous cancer vaccine is not covered by Japan’s public health insurance and is provided as self-funded (private) care.
One course: ¥1,650,000 (incl. tax)
(3 vaccinations per course)
Consultation fee: ¥33,000 (incl. tax)
Medical expense deductions may be available in some situations. Please check with your local tax office.
Frequently Asked Questions
Q. What side effects can occur?
A. The most common reactions are local redness, swelling or firmness at the injection site; these are usually temporary and indicate immune activation. Mild fever can occur. Severe adverse events have not been commonly reported to date, but newly identified side effects may be recognised in the future.
Q. Can it be combined with other treatments?
A. Yes. Combination with radiotherapy, non-lymphocyte-suppressive chemotherapies and immune checkpoint inhibitors may provide synergistic effects in some cases. The final plan will be made with your doctor.
Q. Who is not eligible?
A. Generally ineligible groups include:
• Patients without access to their tumour tissue (FFPE blocks)
• Patients with active autoimmune disease
• Patients in the terminal stage with markedly reduced general condition
• Patients who are pregnant or breastfeeding
Eligibility is finally determined by the treating physician based on clinical judgement.
Q. How is effectiveness assessed?
A. We use imaging (CT, MRI, PET, etc.) and standard oncological criteria. Changes in your general condition and quality of life are also considered.
If you are considering a consultation
If you would like to discuss your condition and explore options in English, please contact us. We support you to make an informed choice aligned with your values and goals.
- This treatment is an unapproved medical product in Japan (not approved under the Pharmaceuticals and Medical Devices Act).
- It is provided as self-funded care (full out-of-pocket) and not covered by public health insurance.
- While reported side effects have generally been limited, new risks may be identified in the future.
- Our clinic (Iwata Neurosurgical Clinic) provides medical care; vaccine manufacturing and development are conducted by the biotech company Cell Medicine, Inc.
You can book at Iwata Neurosurgical Clinic from the link below.
Note: The autologous cancer vaccine is not covered by Japan’s public health insurance and is provided as self-funded (private) care. One course*: ¥1,650,000 (incl. tax) *3 vaccinations per course
Consultant Neurosurgeon
Ryoichi Iwata, MD, PhD
Research focus: Immunotherapies for malignant brain tumours

Receiving the 2020 Japan Neurosurgical Society Encouragement Award
Clinical & research perspective
The immune system comprises innate and adaptive arms. Adaptive immunity recognises tumour antigens and mobilises T and B cells to attack targets. Glioblastoma carries genetic alterations that can yield tumour antigens, yet the disease also employs immune-evasion mechanisms. Rather than focusing on a single antigen, the autologous vaccine uses a patient’s own tumour to induce broader adaptive responses. Combined with maximal safe resection and chemoradiotherapy, it may help extend time to recurrence in selected patients.
Selected publications on brain tumours
Peer-reviewed papers
● Maruyama, M., Nakano, Y., Nishimura, T., Iwata, R., Matsuda, S., Hayashi, M., Nakai, Y. & Nonaka, M. et al. (2021) PC3-Secreted Microprotein Is Expressed in Glioblastoma Stem-Like Cells and Human Glioma Tissues. Biological & Pharmaceutical Bulletin, 44(7), 910–919.
● Iwata, R., Lee, J.H., Hayashi, M., Dianzani, U., Ofune, K., Maruyama, M., Oe, S., Ito, T., Hashiba, T. & Yoshimura, K. et al. (2020) ICOSLG-mediated regulatory T-cell expansion and IL-10 production promote progression of glioblastoma. Neuro-Oncology, 22(3), 333–344.
● Iwata, R., Maruyama, M., Ito, T., Nakano, Y., Kanemura, Y., Koike, T., Oe, S., Yoshimura, K., Nonaka, M. & Nomura, S. et al. (2017) Establishment of a tumour sphere cell line from a metastatic brain neuroendocrine tumour. Medical Molecular Morphology, 50(4), 211–219.
● Iwata, R. & Asai, A. (2016) Treatment of metastatic brain tumour. Nihon Rinsho. Japanese Journal of Clinical Medicine, 74(Suppl 7), 752–756.
● Kim, S-H., Ezhilarasan, R., Phillips, E., Gallego-Perez, D., Sparks, A., Taylor, D., Ladner, K., Furuta, T., Sabit, H., Chhipa, R., Iwata, R. & Nakano, I. et al. (2016) Serine/Threonine Kinase MLK4 Determines Mesenchymal Identity in Glioma Stem Cells in an NF-κB-dependent Manner. Cancer Cell, 29(2), 201–213.
● Ryoichi Iwata, Masato Maruyama, Kohei Ofune, Yosuke Nakano, Soichi Oe, Mikio Hayashi, Shinichi Yoshimura, Masahiro Nonaka & Akio Asai (2018) Relationship between metastatic brain tumours and cancer stem cells. Cytometry Research, 28(1), 13–18. doi:10.18947/cytometryresearch.28.1_13.
● Ryoichi Iwata & Akio Asai (2016) Metastatic brain tumours – treatment overview. Japanese Journal of Clinical Medicine, 74(Suppl 7), 752–756.
Competitive research funding
●科研費 若手研究(B) 2015-2017
B7 familyを標的にした膠芽腫の癌幹細胞に対する新規治療法の開発
役割:研究代表者
●科研費 基盤研究(C) 2015-2018
グリオーマ癌幹細胞を標的とした樹状細胞療法の開発に関する基礎研究
研究代表者:淺井昭雄、役割:研究分担者
●科研費 基盤研究(C) 2017-2020
グリオーマ癌幹細胞特異的に発現する新規バイオマーカーの機能解析
研究代表者:丸山正人、役割:研究分担者
●科研費 基盤研究(C) 2018-2020
グリオーマ幹細胞を用いたがん組織表現型と遺伝子発現への麻酔薬の影響の検討
研究代表者:岩井鉄平、役割:研究分担者
●科研費 基盤研究(C) 2018-2020
グリオーマがん幹細胞におけるOX40シグナルの機能解析
研究代表者:淺井昭雄 役割:研究分担者
●科研費 若手研究 2019-2020
脳転移開始細胞を用いた脳転移の機序解明
役割:研究代表者
●科研費 基盤研究(C) 2020-2022
内向き整流Kチャネルを基軸としたグリオーマ浸潤メカニズムの解明
研究代表者:吉村晋一、役割:研究分担者
●公益財団法人 赤枝医学研究財団 研究助成金
脳転移開始細胞を標的とした新規がん治療法の開発
Patent
Nitrogen-containing compounds, compositions containing nitrogen-containing compounds, and predictive markers for tumour malignancy
Inventors: Mikiō Hayashi, Yuki Ikeda, Ryoichi Iwata
Contact us
If you prefer messaging, feel free to contact us via our official LINE account.
This page is for general information and does not replace individual medical advice. Suitability and decisions about care will be made after clinical assessment.